What Is the Best Medication for Diverticulitis?
Diverticulitis is a relatively rare condition in the population at large, but it becomes more common as people get older. In fact, according to the National Institutes of Health (NIH), only 30% of adults between 50-59 have the condition, but that figure increases to 70% for adults over the age of 80. While there are some lifestyle changes that can potentially prevent the condition, most of the time it requires specific medication prescribed by a gastroenterologist to fully treat.
What Is Diverticulitis?
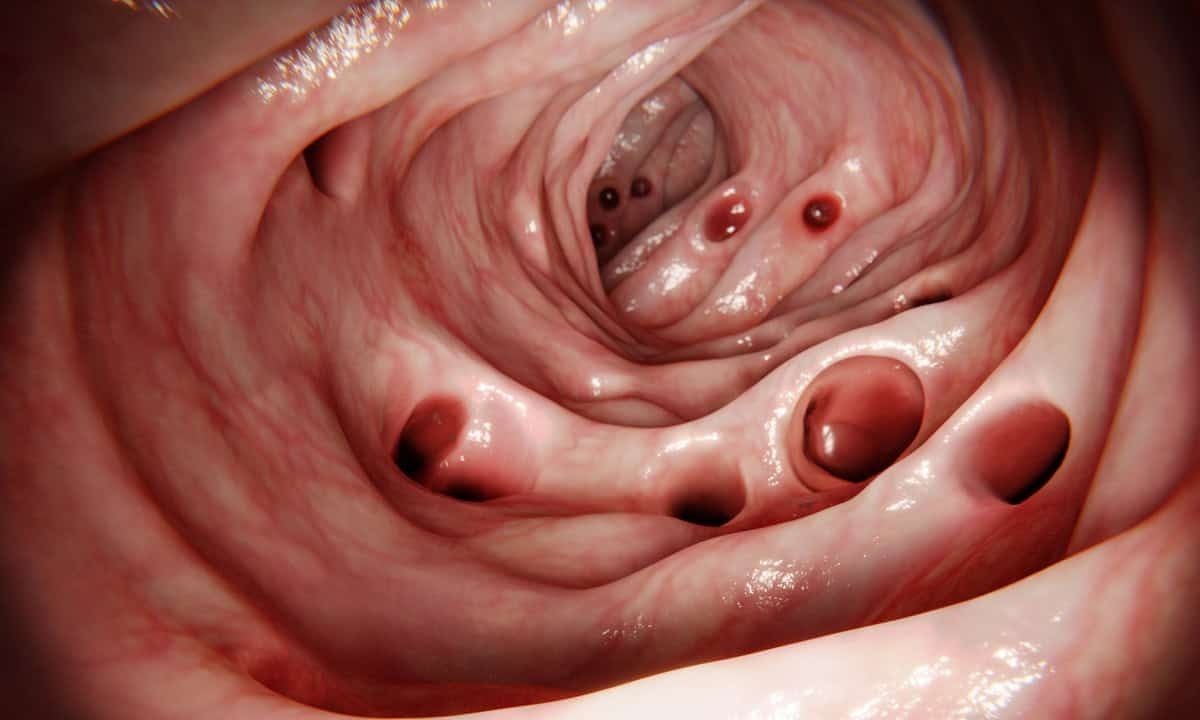
Diverticulitis is actually a complication of another condition called diverticulosis. In diverticulosis, the person has developed a series of small pouches called diverticula along the lining of the large intestine. Though these pouches can form on any part of the colon wall, they are more likely to appear in the sigmoid colon just prior to the rectum. It is unclear why diverticula develop in the first place, but a widely accepted theory is that physical pressure on the colon (from straining to pass stools, for example) causes weak spots to bulge out and form a pouch.
The presence of a diverticulum in the colon isn’t necessarily a cause for concern; after all, many people have them and are totally unaware. But the fact that they are pouches in the colon wall means that bacteria can potentially get trapped and begin multiplying. When this happens, the diverticula can become infected, which is the condition known as diverticulitis. Together, diverticulosis and diverticulitis are often collectively referred to as diverticular disease given how closely related they are.
Diverticulitis is typically classified as either asymptomatic, acute uncomplicated, acute complicated, or chronic. In acute uncomplicated diverticulitis, the diverticula are inflamed and possibly infected, but the condition ends up being fairly easy to treat. With the complicated diverticulitis variety, as the name implies, there are additional complications like bleeding, intestinal obstruction, or swelling. The condition can also be chronic, with a pattern of inflammation and infection that never fully resolves.
Symptoms of Diverticulitis
Some people with diverticulitis won’t have any symptoms at all, and the diverticula present in the colon won’t need to be addressed by a healthcare provider. For chronic and acute diverticulitis, however, there a number of possible symptoms that can emerge that vary from person to person:
- Abdominal pain: Often experienced in the lower lower left side of the abdomen, the pain is typically severe and presents rather suddenly. It can also be more mild yet increase in severity over a period of days.
- Changes in bowel habits: Inflammation in the wall of the colon naturally has implications for the digestive process; many people report a change in the frequency and consistency of bowel movements. Common gastrointestinal symptoms like bloating, constipation, and diarrhea are also normal.
- Feeling ill: In cases where an infection has begun, there are related symptoms that can lead to general feelings of illness; examples include nausea, vomiting, fever, and chills.
- Bleeding: Though not as common, diverticular bleeding can occur in severe cases with a significant infection or other complications.
Diverticulitis Complications
While diverticulosis is somewhat common in the United States among older adults, diverticulitis is more rare and only affects 4-15% of those with diverticula present in the colon. Of this group of patients, about 15% develop complications that can range from relatively minor to life-threatening. Below are some of the complications patients may experience:
- Abscess: When an infection occurs in a diverticulum, it can become essentially walled off from the rest of the colon. This can cause pus to build up and abscess to form. Collections of these infected sacs can cause severe abdominal pain as well as fever, chills, and swelling.
- Peritonitis: The peritoneum is a lining along the inner wall of the abdomen that can be a major issue if it becomes infected (peritonitis). This can happen if the wall of the colon is broken in some way, including from an abscess that ruptures and leaks pus or other harmful substances into the abdominal cavity. Widespread inflammation of the abdominal cavity is considered a medical emergency that requires rapid treatment.
- Perforation: Depending on the number and size of the diverticula, the colon wall can become more susceptible to tears or perforations that can lead to peritonitis or other problems.
- Fistula: A fistula is an abnormal connection that forms between the colon and another organ, such as the bladder, vagina, or skin. Fistulas are often the result of inflammation and infection spreading from a diverticulum.
- Obstruction: An intestinal obstruction occurs when the colon is partially or completely blocked. This can result from chronic inflammation and scarring (strictures) caused by recurrent episodes of diverticulitis.
Diagnosis and Treatment
Before treatment can be administered, diverticulitis must be diagnosed by a gastroenterologist. This is often done through a series of blood tests and imaging tests like a colonoscopy, CT scan, or X-ray. Once the diagnosis is confirmed, the treatment will be dependent on the severity of the condition as well as whether it is chronic or acute. For mild cases, the condition may be dealt with via antibiotics and changes to one’s diet; the clear liquid diet, that involves broth and juices, is one common recommendation that can promote the healing process.
For more severe or chronic cases, there are a variety of other interventions that may be necessary, including surgery. Bowel resection, for instance, may be required to remove the affected segment of the colon (colectomy). In some situations a colostomy bag (usually temporary) is used to divert waste while the bowels rest. This also typically requires intravenous hydration and nutrition until it is safe to gradually reintroduce solid foods into the diet.
Medication Options
Diverticulitis can’t really be cured in the traditional sense, but the symptoms can be managed until it is eventually resolved. In addition to dietary changes, there are a number of medications that can either treat the infection or relieve symptoms like abdominal pain. Below are some of the best medications for treating diverticulitis:
Mild to moderate or uncomplicated
- Metronidazole: antibiotic that is effective against an infection of anaerobic bacteria
- Ciprofloxacin: usually combined with metronidazole to cover a wide range of bacteria types
- Amoxicillin-clavulanate: a broad-spectrum antibiotic that covers both aerobic and anaerobic bacteria and is also sometimes used with metronidazole
- Hyoscyamine: an antispasmodic medication used to reduce colon spasms
Severe or complicated
- Piperacillin/tazobactam: a more potent antibiotic that has broad coverage of bacteria for complicated diverticulitis
- Meropenem: another antibiotic to treat an infection that is also administered via intravenous tube
- Acetaminophen: since nonsteroidal anti-inflammatory drugs (NSAIDs) can potentially increase the risk of a bowel perforation, painkillers like acetaminophen are used instead
The particular combination of medications will be determined on a case-by-case basis, but almost all treatments involve an antibiotic to treat the infection and other medications for relief of symptoms. The gastroenterologist may also recommend fiber supplements for some patients, but they shouldn’t be taken without speaking with the doctor. Some people have also suggested probiotics as another option, but there is so far little evidence of their effectiveness.
Contact Cary Gastroenterology
Even though the risk of diverticulitis is pretty low until we start getting older, the condition highlights the need for mindfulness related to digestive health. Our dietary and lifestyle habits can have a major effect on the gastrointestinal tract, and good health often means taking the time to investigate potential problems. If you have been experiencing any of the symptoms noted above, it may be time to see a gastroenterologist like one of the board-certified physicians at Cary Gastro. Please contact us today to request an appointment.