What Is MAFLD?
Metabolic dysfunction-associated steatotic liver disease (MAFLD) is the complex name for a condition that is rapidly becoming a significant health concern worldwide. Affecting an estimated 25% of the global population, MAFLD is closely linked to the rising prevalence of obesity, type 2 diabetes, and metabolic syndrome. This condition, previously known as non-alcoholic fatty liver disease (NAFLD), is now recognized as the most common chronic liver disease in many parts of the world. As lifestyles become increasingly sedentary and diets high in processed foods become more prevalent, understanding MAFLD and its implications for overall health has never been more crucial.1
A New Name for a Common Liver Condition
In 2020, a significant change occurred in the field of hepatology when experts proposed renaming non-alcoholic fatty liver disease (NAFLD) to metabolic dysfunction-associated steatotic liver disease (MAFLD). This shift represents more than just a change in terminology; it reflects an evolution in our understanding of this common liver condition. The new name moves away from defining the disease by what it is not (non-alcoholic) and instead focuses on its association with metabolic factors. This change in perspective is expected to improve diagnosis, guide more targeted research, and potentially lead to better treatment strategies for patients.
The Basics of MAFLD
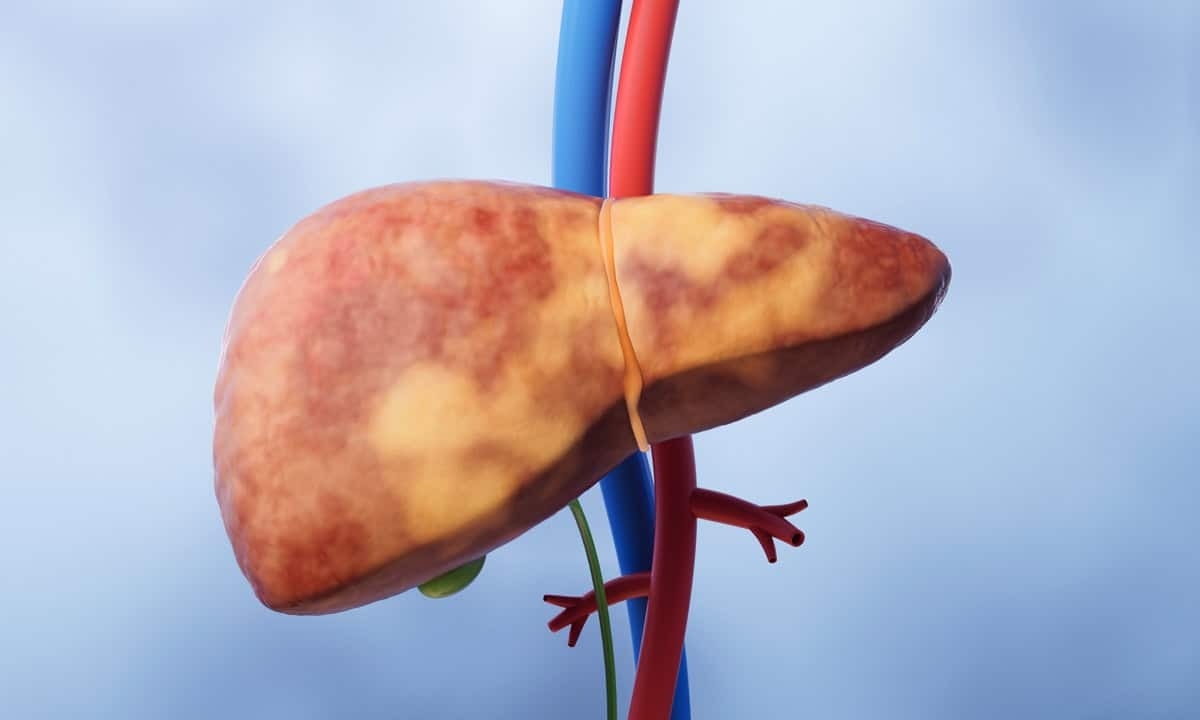
It is estimated that MAFLD affects about 25% of the global population with increasing incidence worldwide, particularly in Western countries and urban areas of developing nations. The condition is more prevalent among individuals with risk factors such as obesity, type 2 diabetes, or metabolic syndrome. MAFLD is characterized by excessive fat accumulation in the liver (hepatic steatosis), and it is closely linked to insulin resistance, dyslipidemia, and metabolic dysfunction. The accumulation of lipids—particularly triglycerides—in liver cells can lead to inflammation and potential liver damage over time.
MAFLD encompasses a spectrum of liver conditions, ranging from simple steatosis to more severe forms. As the disease progresses, it can develop into metabolic dysfunction-associated steatohepatitis (MASH, previously known as NASH), where inflammation and liver cell damage become more prominent. In some cases, if left unchecked, MAFLD can advance to liver fibrosis, where scar tissue begins to replace healthy liver tissue. The most severe progression can lead to cirrhosis, a condition characterized by extensive scarring that impairs liver function, and in some cases, even hepatocellular carcinoma (liver cancer).
The exact causes of MAFLD are not fully understood, but several factors contribute to its development. At its core, MAFLD occurs when the liver accumulates more fat than it can process effectively. This can happen when too much fat enters the liver, when the liver produces too much fat on its own, or when the liver has trouble breaking down or exporting fat. Insulin resistance, a condition where the body’s cells don’t respond well to insulin, often plays a key role in this process. It can disrupt how the body handles fats and sugars, leading to more fat buildup in the liver. Over time, this excess fat can cause inflammation and damage to liver cells, potentially leading to more serious liver problems.2
Risk Factors for MAFLD
The development of MAFLD is influenced by a complex interplay of genetic, metabolic, and environmental factors. While the exact causes can vary from person to person, certain risk factors have been consistently associated with a higher likelihood of developing MAFLD. Understanding these risk factors is crucial for identifying individuals at higher risk and implementing preventive strategies. Here are the primary risk factors associated with MAFLD:
- Obesity: Excess body weight, especially visceral adiposity (fat around the abdominal organs), is strongly linked to MAFLD. A high body mass index (BMI) increases the risk of fat accumulation in the liver.
- Type 2 diabetes: Insulin resistance, a hallmark of type 2 diabetes, plays a significant role in the development of MAFLD. It affects the body’s ability to regulate glucose and lipid metabolism, leading to increased fat storage in the liver.
- Metabolic syndrome: This cluster of conditions, including high blood pressure, high blood sugar, excess body fat around the waist, and abnormal cholesterol levels, significantly increases the risk of MAFLD.
- Dyslipidemia: Abnormal blood lipid levels, particularly high triglycerides and low high-density lipoprotein (HDL) cholesterol, are associated with an increased risk of MAFLD.
- Age and gender: While MAFLD can occur at any age, it becomes more common as people get older. Some studies suggest that men may be at slightly higher risk than women, although this difference tends to decrease after menopause.
- Diet: Diets high in processed foods, saturated fats, and added sugars have been associated with an increased risk of MAFLD. Excessive consumption of fructose, often found in sugar-sweetened beverages, may also add to the risk.
- Physical activity: A lack of regular physical activity is a significant risk factor for MAFLD, independent of its effects on body weight.
- Certain medications: Some medications, such as corticosteroids, tamoxifen, and certain antipsychotics, can increase the risk of developing MAFLD.
- Other conditions: Conditions such as polycystic ovary syndrome (PCOS), sleep apnea, and hypothyroidism have also been associated with an increased risk of MAFLD.
Diagnosis and Treatment
The diagnosis of MAFLD typically involves a combination of clinical evaluation, laboratory tests, and imaging studies. Doctors may perform a physical examination to check for an enlarged liver, conduct blood tests to assess liver function and metabolic health, and use imaging techniques like ultrasound, CT, or MRI to detect liver fat. In some cases, specialized tests like magnetic resonance elastography (FibroScan®) may be used to assess liver stiffness, which can be an indicator of fibrosis. While less common now due to non-invasive alternatives, a liver biopsy might be recommended in certain situations to confirm the diagnosis or assess the severity of liver damage.
Once diagnosed, the treatment options for MAFLD tend to focus on managing the underlying metabolic dysfunctions and preventing further liver damage. The approach is typically multifaceted and individualized based on the severity of the disease, associated conditions, and overall health status of the patient. Here are the main components of MAFLD treatment:
- Lifestyle modifications: Making lifestyle modifications is typically the first-line approach to treatment. Key changes include weight loss, dietary improvements, and increased physical activity. There is some evidence that even a modest weight reduction of 5-10% can significantly improve liver health. Patients are advised to follow a balanced diet low in saturated fats, simple carbohydrates, and fructose. Regular exercise helps improve insulin sensitivity and reduce liver fat accumulation. These lifestyle changes not only target liver health but also improve overall metabolic function.
- Management of metabolic conditions: Treating associated conditions like type 2 diabetes, hypertension, and dyslipidemia is crucial. This may involve the use of medications to improve insulin sensitivity, such as metformin, when appropriate. Managing these related conditions can also have a positive impact on liver health.
- Medications for liver health: While there are no FDA-approved medications specifically for MAFLD, some drugs are being studied for their potential benefits. Vitamin E supplementation has shown promise for non-diabetic patients with MAFLD in certain cases. Additionally, medications like pioglitazone may be considered in specific situations under medical supervision.
- Liver-directed therapies: For patients with advanced MAFLD, particularly those who have developed cirrhosis, treatments focused on managing complications may be necessary. In severe cases where liver function is significantly compromised, liver transplantation might be considered as a last resort.3
Cary Gastro for Digestive Health
While MAFLD is a serious condition, early detection and appropriate management can significantly improve outcomes and quality of life. Many of the symptoms and risk factors associated with MAFLD are common to various metabolic and liver disorders, making professional evaluation crucial. If you have concerns about your liver health, especially if you have any of the risk factors mentioned above, it’s a good idea to consult with a gastroenterology specialist. The experienced physicians at Cary Gastro are equipped to provide comprehensive evaluation and personalized treatment plans for MAFLD and other liver conditions. Don’t hesitate to reach out to Cary Gastro with any questions or to request an appointment.
1https://pubmed.ncbi.nlm.nih.gov/36761200/
2https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10583766/
3https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9747889/