Understanding Peptic Ulcer Disease
Stomach pain and abdominal discomfort are among the most common gastrointestinal complaints, and they affect countless numbers of people worldwide. While occasional discomfort is normal, persistent or severe pain can indicate a more serious condition. One such condition is peptic ulcer disease, a prevalent digestive disorder characterized by open sores in the lining of the stomach or the duodenum. These ulcers can cause significant discomfort and, if left untreated, may lead to serious complications.
What Is Peptic Ulcer Disease?
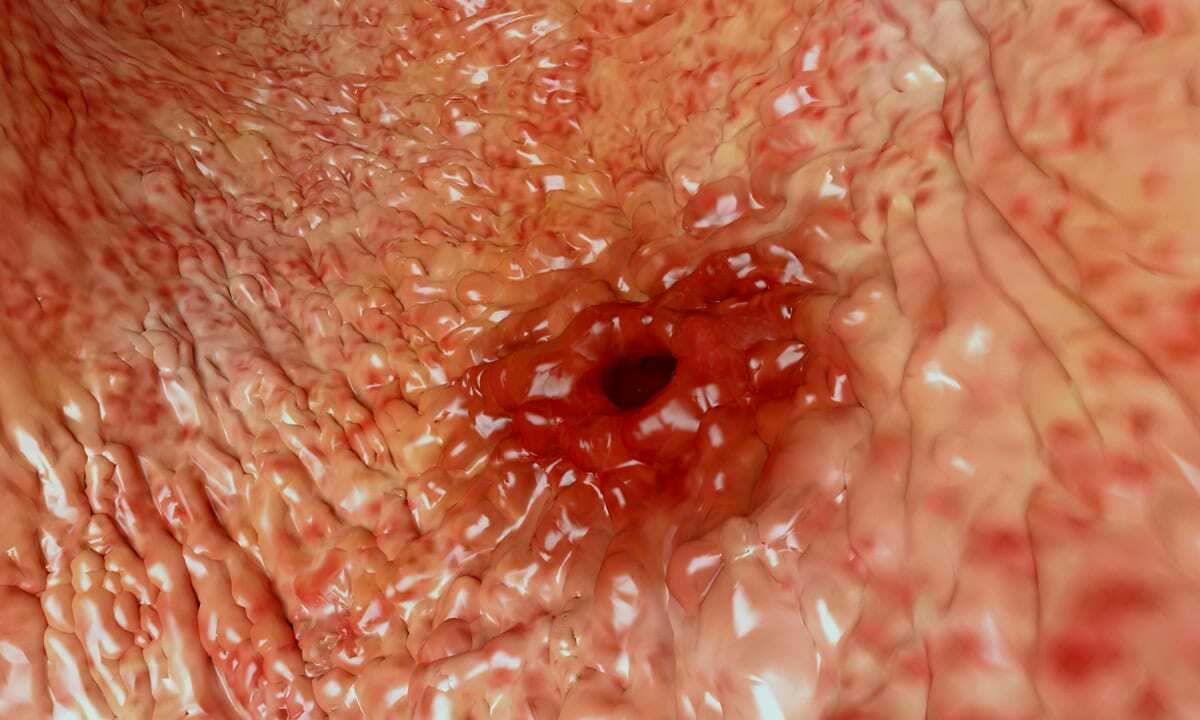
Peptic ulcer disease is a common digestive disorder characterized by open sores (ulcers) that develop in the lining of the stomach (gastric ulcers) or the first part of the small intestine, called the duodenum (duodenal ulcers). Both the stomach and duodenum are lined with a protective mucus layer (mucosa) that shields them from the harsh acidic environment necessary for digestion. When this protective barrier is compromised, the acid can erode the underlying tissue, resulting in an ulcer.
The prevalence of peptic ulcer disease varies across different populations and age groups, but it tends to be more common in older adults, with a peak incidence in people between 55 and 65 years old. In the United States alone, it's estimated that about four million people have active peptic ulcers, and nearly 350,000 new cases are diagnosed each year.
The ulcers themselves can range from mild to severe and may cause typical gastrointestinal symptoms or sometimes won’t present with symptoms at all. Indeed, this variability in presentation can sometimes lead to delayed diagnosis and treatment as other conditions are ruled out. The impact of peptic ulcer disease extends beyond physical symptoms, and it can significantly affect a person's quality of life, daily activities, work productivity, and overall well-being.1
Symptoms of Peptic Ulcer Disease
Peptic ulcer disease can manifest in various ways, and the severity of symptoms often depends on the ulcer’s location and the individual’s overall health. While some people with peptic ulcers may experience no symptoms at all, others might suffer from significant discomfort. It’s important to recognize these symptoms early, as prompt diagnosis and treatment can prevent more serious complications. The following list outlines the most common symptoms associated with peptic ulcer disease:
- Abdominal pain: The most common symptom is a burning or gnawing pain in the abdomen, typically between the breastbone and navel. This pain may be worse when the stomach is empty, occur at night, and temporarily subside after eating or taking antacids. It can last for minutes to hours and may come and go for several days, weeks, or months.
- Bloating: Patients often experience a feeling of bloating or swelling in the abdominal area, which can be uncomfortable and may affect appetite.
- Heartburn: A burning sensation in the chest may occur, and this can sometimes be mistaken for acid reflux or gastroesophageal reflux disease (GERD).
- Nausea: Feeling sick to your stomach is common, and in some cases, it may be accompanied by vomiting.
- Loss of appetite: Individuals with peptic ulcers may experience a reduced desire to eat due to discomfort or fear of triggering pain.
- Unexplained weight loss: Some patients may lose weight without trying, possibly due to reduced appetite or changes in eating habits to avoid discomfort.
- Indigestion (dyspepsia): General upper abdominal discomfort is common, often described as a feeling of fullness or burning that may be relieved by eating, drinking, or taking antacids.
- Fatty food intolerance: Many people with peptic ulcers experience discomfort or pain after eating fatty or greasy foods.
In more serious cases, symptoms may also include vomit that looks like coffee grounds, which generally indicates bleeding in the digestive tract. Another possible indicator of gastrointestinal bleeding is passing dark, tarry stools. Persistent abdominal pain that is especially severe or sharp could be evidence of a perforation or another serious complication; this requires rapid medical evaluation.
What Causes Peptic Ulcers?
Peptic ulcers develop when the delicate balance between stomach acid and the protective mucus layer in the digestive tract is disrupted. This imbalance allows the stomach acid to erode the lining of the stomach or duodenum, leading to the formation of ulcers. While stress and spicy foods were once thought to be the primary culprits, modern medical research has identified two main causes of peptic ulcer disease:
- Helicobacter pylori: An infection of the H. pylori bacterium is the most common cause of peptic ulcers overall. This bacteria is well-suited to the harsh, acidic environment of the stomach, and over time it can weaken the protective mucus coating of the stomach and small intestine. When weakened, acid can reach the more sensitive layers of the stomach lining and lead to the sores known as ulcers. Such infections are often acquired in childhood and can persist for years without symptoms before causing ulcers.
- NSAIDs: The second most common cause of peptic ulcers is the regular use of NSAIDs (nonsteroidal anti-inflammatory drugs) like aspirin, ibuprofen, and naproxen. These medications can irritate or inflame the stomach and intestinal lining, making it more vulnerable to acid damage. NSAIDs reduce the production of prostaglandins, substances that help protect the stomach lining, thereby increasing the risk of ulcer formation. The risk increases with higher doses and longer duration of NSAID use.
While these are the primary causes, there are other factors that can increase the risk of developing peptic ulcers or exacerbate existing ones. In addition to lifestyle habits like smoking or excessive alcohol consumption, there are some medical conditions that also make ulcers more likely. One relatively rare condition is Zollinger-Ellison syndrome, a disorder that causes tumors in the pancreas and duodenum, leading to increased stomach acid production.2
Diagnosis and Treatment
The diagnosis of peptic ulcer disease follows many of the conventions involved in diagnosing other gastrointestinal issues. This typically involves a combination of medical history review, physical examination, and diagnostic tests. One of the go-to imaging tests is an upper endoscopy (also known as esophagogastroduodenoscopy or EGD), where a thin, flexible tube with a camera is inserted through the mouth to examine the esophagus, stomach, and duodenum. During this procedure, a biopsy may be taken for further analysis.
For ulcers thought to be related to the H. pylori bacteria, blood tests, stool tests, or urea breath tests can be used to detect the presence of the bacteria. Another diagnostic tool is the upper gastrointestinal series (upper GI), also known as a barium swallow. This X-ray test involves drinking a white liquid containing barium, which coats the digestive tract and makes ulcers visible on X-rays.
Treatment for peptic ulcer disease depends on the underlying cause and severity of the condition. If a bacterial infection is present, a combination of antibiotics and bismuth salts is prescribed to eradicate the bacteria. Acid-suppressing medications, such as proton pump inhibitors (PPIs) like omeprazole, esomeprazole, or pantoprazole, or histamine blockers (H2 blockers) like famotidine, are used to reduce stomach acid production and promote healing.
Over-the-counter antacids can also provide quick relief from symptoms by neutralizing stomach acid.
Cytoprotective agents like misoprostol may be prescribed to help protect the lining of the stomach and small intestine. If NSAID use is the cause of the ulcer, the medication may need to be stopped or replaced with an alternative like acetaminophen. In addition to medical treatments, lifestyle modifications can help manage peptic ulcer disease. These include avoiding triggers such as alcohol, tobacco, and excessive coffee consumption, eating smaller, more frequent meals, managing stress through relaxation techniques or counseling, and avoiding lying down immediately after meals.
Most peptic ulcers heal within a few months of starting treatment. However, it’s essential to complete the full course of prescribed medications, even if symptoms improve, to ensure complete healing and prevent recurrence. Follow-up appointments with your gastroenterologist are important to confirm that the ulcer has healed and to discuss any ongoing management strategies.
Request an Appointment
Having a stomach ulcer can be pretty unpleasant, but it’s also fortunately not too burdensome to treat, provided that the treatment isn’t avoided for too long. However, many of the common symptoms are shared by various other gastrointestinal problems. If you have been experiencing any of the symptoms noted above, you might benefit from connecting with a gastroenterologist like the highly experienced physicians at Cary Gastro. Contact us today for any questions or to request an appointment.
1https://www.niddk.nih.gov/health-information/digestive-diseases/peptic-ulcers-stomach-ulcers
2https://www.ncbi.nlm.nih.gov/books/NBK534792/