Invisible Blood in Stool: Causes, Testing, and What It Means for Your Health
Digestive health issues don’t always come with obvious symptoms. Visible blood in the stool may appear as red streaks, dark discoloration, or redness on the toilet paper, but not all gastrointestinal bleeding is easy to detect. In some cases, small amounts of blood are present without any noticeable change in appearance. This hidden blood, medically known as occult blood, serves as an important warning sign for various digestive conditions ranging from minor irritations to more serious issues. Because this type of bleeding typically causes no symptoms on its own, specialized screening tests play a crucial role in detecting potential problems early, when treatment is often most effective.1
Common Causes of Occult Blood in Stool
Because the digestive tract contains an extensive network of blood vessels running through its walls, any number of conditions can potentially lead to minor bleeding. Occult blood can originate from any part of the digestive tract and eventually become mixed with stool in the colon. Some causes of occult bleeding resolve with minimal intervention, while others signal potentially serious conditions that require prompt medical attention. Multiple factors—including age, medication use, family history, and underlying health conditions—influence which causes are most likely in any individual case:
- Colorectal polyps: These small growths on the lining of the colon or rectum often bleed intermittently, releasing tiny amounts of blood that mix with stool. Most polyps are benign, but some can gradually develop into colorectal cancer over time. Detecting polyps early through occult blood testing helps prevent cancer development.
- Colorectal cancer: Cancerous colorectal tumors cause occult bleeding through several mechanisms. They form new, fragile blood vessels that bleed easily, and as tumors expand, they can ulcerate the intestinal lining, leading to slow, chronic bleeding. This bleeding often remains occult until the disease advances, making regular screening crucial for early detection.
- Inflammatory bowel disease: Conditions like Crohn’s disease and ulcerative colitis frequently cause microscopic bleeding due to chronic inflammation of the intestinal lining. This inflammation creates small ulcerations and increases the fragility of digestive tract tissue, resulting in ongoing, low-level bleeding.
- Peptic ulcers: Erosions in the stomach or duodenal lining can develop into ulcers that penetrate blood vessels, causing slow bleeding. By the time this blood passes through the digestive system, it typically becomes occult and detectable only through testing.
- Hemorrhoids and anal fissures: While hemorrhoids and anal fissures often produce visible bleeding, they usually bleed minimally, resulting in blood amounts too small to be noticed. These sources of bleeding originate in the rectum or anal canal.
- Diverticulosis: Small pouches (diverticula) that form in the colon wall can become inflamed or irritated, causing minimal bleeding. When numerous diverticula are present, this can lead to persistent occult blood in stool.
- Medication effects: Non-steroidal anti-inflammatory drugs (NSAIDs) like aspirin, ibuprofen, and naproxen can irritate the digestive tract lining and interfere with blood clotting. Blood-thinning medications prescribed for heart conditions may also contribute to occult bleeding by preventing normal clotting when minor injuries occur.2
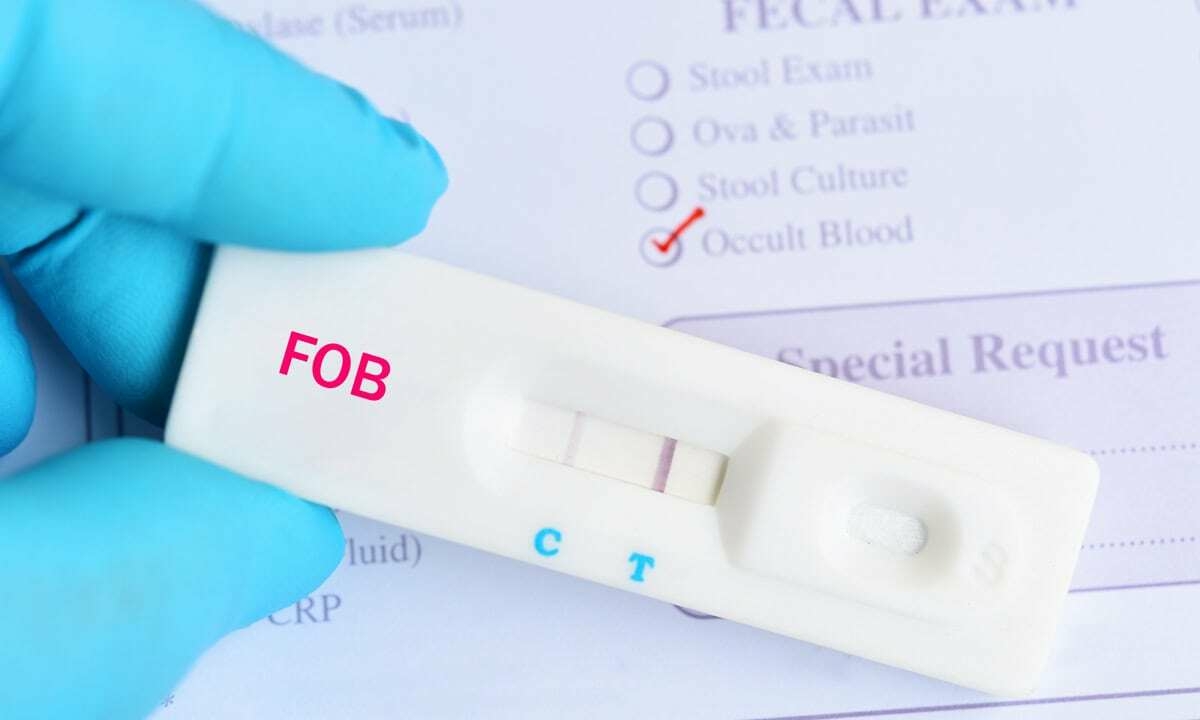
Fecal Occult Blood Tests: How They Detect Hidden Blood
Laboratory testing provides the only reliable method for detecting occult blood in stool. Several different testing options exist, each with specific advantages and limitations. These tests vary in their detection methods, sensitivity, and requirements for patient preparation. Healthcare providers typically select the most appropriate test based on the patient’s specific risk factors, medical history, and screening needs:
- Guaiac-based fecal occult blood test (gFOBT): This traditional test uses guaiac, a plant-based substance that changes color when exposed to blood components. The test detects a component of hemoglobin called heme, which gives red blood cells their oxygen-carrying ability. Because gFOBT reacts to any heme source, patients must follow dietary restrictions before testing, avoiding red meat, certain vegetables, and vitamin C supplements to prevent false results.
- Fecal immunochemical test (FIT): Also called an immunochemical fecal occult blood test (iFOBT), this newer method specifically detects human hemoglobin protein using antibodies. Unlike gFOBT, the FIT doesn’t react to non-human blood or other compounds, eliminating the need for dietary restrictions before testing. This improved specificity reduces false positives and makes the test more convenient for patients to complete.
- FIT-DNA test (Cologuard®): This advanced screening method combines FIT testing with analysis of altered DNA markers associated with colorectal cancer and precancerous polyps. By examining both blood and DNA biomarkers, this test offers enhanced sensitivity for detecting certain types of lesions. It requires a single stool sample and no dietary restrictions, though it typically costs more than standard occult blood tests.
- Fecal occult blood testing for diagnostic purposes: Beyond routine screening, healthcare providers often use these tests to evaluate specific symptoms like abdominal pain, unexplained weight loss, or changes in bowel habits. In these cases, positive results generally lead to prompt follow-up with direct visualization tests like colonoscopy.
Fecal occult blood tests play a crucial role in colorectal cancer screening programs worldwide. The American Cancer Society recommends regular screening beginning at age 45 for people at average risk, with earlier screening for those with family history or other risk factors. When used at recommended intervals, these tests help detect potential problems early, significantly improving treatment outcomes.
The Fecal Occult Blood Test Procedure
Most fecal occult blood testing occurs through at-home collection kits that patients receive from their healthcare providers. The process involves collecting small stool samples according to the instructions provided with the kit. For gFOBT and standard FIT tests, this typically means using an applicator to take tiny samples from different areas of the stool and applying them to designated cards or tubes. The collection usually spans two to three bowel movements over several days to ensure accurate results.
After collection, patients seal the samples in the provided envelopes and return them to their healthcare provider or laboratory for analysis. The process is simple and designed to be completed privately at home, with results typically available within one to two weeks. A negative result usually indicates no active bleeding, while a positive result often leads to follow-up testing, such as a colonoscopy, to determine the source of bleeding. Proper sample handling directly impacts test accuracy, so patients are encouraged to follow instructions closely.3
Schedule an Appointment With Cary Gastro
The presence of occult blood in stool should never be ignored, as it can be an early indicator of conditions ranging from minor irritations to more serious digestive disorders. If you’re experiencing digestive symptoms or have risk factors for colorectal cancer, regular screening is an important part of maintaining your digestive health. The gastroenterologists at Cary Gastro provide comprehensive evaluation, testing, and treatment for a wide range of digestive conditions. Contact us today to schedule an appointment and take a proactive step toward protecting your digestive health.
1https://www.cancer.gov/publications/dictionaries/cancer-terms/def/fecal-occult-blood-test
2https://www.ncbi.nlm.nih.gov/books/NBK563143/
3https://www.mskcc.org/cancer-care/patient-education/fecal-occult-blood-test