What is Endoscopic Retrograde Cholangiopancreatography (ERCP)?
The gastrointestinal tract is a complex system of organs and tissues that is crucial for our ability to get energy from the food we eat. When something goes wrong, however, it can sometimes be difficult to determine the cause. This is especially true when the problem seems to be related to the pancreatic or biliary ductal systems. These biological systems rely on substances moving smoothly through small ducts, and to investigate those ducts, a unique type of imaging test is required: endoscopic retrograde cholangiopancreatography (ERCP).
Overview of ERCP
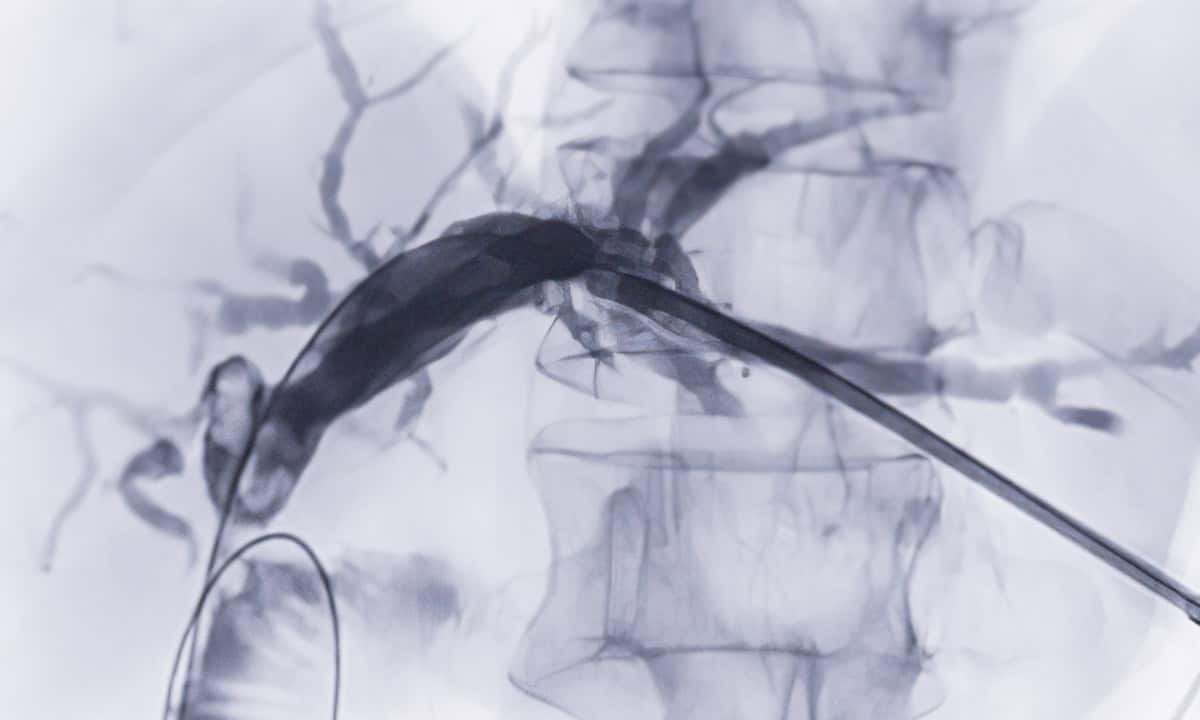
ERCP is a specialized medical procedure primarily used to diagnose and treat disorders of the bile ducts, gallbladder, and pancreas. ERCP is somewhat unique because it uses a combination of endoscopy and fluoroscopy to access and examine these structures. Endoscopy refers to the use of an endoscope, which is a flexible tube with camera and surgical tools mounted on the end. Fluoroscopy refers to the use of X-rays to generate real-time images of the part of the body’s interior in question.
The biliary system (or biliary tree as it is sometimes called) plays an important role in the digestive process because of how it introduces bile into the digestive tract. Bile itself is produced by liver cells and is partly collected by the gallbladder before moving through the common bile duct. Bile is then combined with digestive enzymes from the pancreatic duct via the ampulla of Vater, a structure adjacent to the duodenum. These digestive “juices” enter the digestive tract through this first part of the small intestine.
Naturally the biliary system isn’t easy to access since it is deep inside the abdominal cavity surrounded by vital organs. A gastroenterologist trying to diagnose a related condition can only learn so much from evaluating symptoms and performing a physical exam, so it is sometimes necessary to get a more in-depth look. ERCP allows detailed evaluation of the biliary ducts without requiring an invasive surgery or incisions that require a long recovery time. Instead, the ERCP procedure can be done on an outpatient basis over a relatively short time.1
Conditions that Might Require an ERCP
Given the capabilities of an endoscopic procedure, an ERCP procedure can be used to diagnose and/or treat conditions related to the biliary system. While noninvasive tests like magnetic resonance cholangiopancreatography (MRCP) or endoscopic ultrasound may be used first, an ERCP is often relied upon when one or more of the ducts has been narrowed or blocked. Below are some examples of conditions that make prompt use of ERCP:
- Gallstones: One of the most common reasons for ERCP is the presence of a gallstone in the common bile duct (choledocholithiasis). Gallstones, and bile duct stones more generally, are hard, jagged concretions that typically form when there is an imbalance in the substances that comprise bile.2 When a gallstone is sufficiently large enough, it can become lodged in the bile duct and cause abdominal pain and a variety of other symptoms. If it doesn’t break up on its own, it will need help from a doctor to remove it.
- Bile duct infection: Another relatively common reason for an ERCP procedure is a bacterial infection of the bile ducts (cholangitis). Usually brought on by either a bile duct blockage or stricture, such an infection can cause inflammation and a number of other symptoms. ERCP can be used to identify an infection and potentially drain infected bile from the area.
- Strictures: Inflammation due to an infection can also cause a narrowing of the bile ducts called a stricture. Even if the bile duct isn’t actually being blocked, a stricture can substantially reduce the flow enough to cause digestive problems.
- Pancreatitis: Pancreatitis is the term for inflammation of the pancreas; like with a number of other biliary problems, pancreatitis is often caused by a gallstone-related blockage in the bile ducts but it can also be related to trauma or a prior surgery.
- Tumors: ERCP can also be used in the process of diagnosing and staging both cancerous and benign tumors in the biliary system. In fact, ERCP is often one of the best tools for determining the nature of the tumor and what kind of treatment it will require.
- Jaundice: Jaundice refers to the state of having a yellowish or greenish pigmentation of the skin and eyes. While often associated with liver dysfunction or liver failure, obstructive jaundice can also indicate a blockage in the biliary tract. ERCP can be used to rule out the liver as the cause.
How Does the Procedure Work?
When a doctor has determined that an ERCP procedure is necessary for either diagnosis or treatment, it is performed in a similar way as other endoscopic procedures. After intravenous sedation, the patient is positioned on their left side or back. The endoscopist then feeds the flexible tube down the esophagus of the patient; typically a mouth guard and/or a numbing agent are used to ease the passage of the tube. Once the endoscope reaches the area, a catheter is extended into the biliary system.
This catheter is positioned so it can be extended into the ampulla of Vater, the place where bile enters the digestive tract. A contrast dye is injected through the catheter so that it can be distributed throughout the biliary system. This allows X-ray images (fluoroscopy) to show a clear visualization of the biliary ducts and any obstructions that may be present. In many cases, the endoscopist will only be able to decide on the next course of action once they have access to the X-ray images.
Depending on what the doctor finds, there are several different interventions that can be attempted if an abnormality is identified. Below are some common options for next steps:
- Stone removal: The endoscope has a series of surgical tools mounted on the end that may be able to break up or remove a stone causing a blockage.
- Stent placement: A small tube, called a stent, can also be inserted into a bile duct that has been blocked or narrowed. The insertion of the stent allows bile to flow freely again.
- Dilation: In the case of a stricture, another option is to use a special balloon to inflate and dilate the duct. This essentially widens the duct so that bile can flow more freely.
- Biopsy: In situations where an abnormality is detected, the endoscopist can also take a tissue sample for a biopsy.
Possible Post-ERCP Side Effects
As effective as ERCP is for diagnosing and treating conditions of the biliary tract, it isn’t without any risk. For instance, even though ERCP can be used to treat acute or chronic pancreatitis, it can also potentially cause pancreatitis as well; this can happen if the endoscope or catheter irritates the tissues in the area. Additionally, there are several other possible side effects of the ERCP procedure:
- bleeding or perforation of the gastrointestinal tract
- sore throat or difficulty swallowing
- abdominal pain
- bloating due to air added to the stomach during the procedure
- nausea
Cary Gastroenterology for Digestive Health
Ideally nobody would need ERCP, but research shows that about 10-15% of the adult population in the United States will have a gallstone obstruct their biliary tract at some point in life.3 At Cary Gastro, our elite team of healthcare professionals is dedicated to helping patients get the care they need regardless of the problem. If you have been experiencing any of the symptoms noted above and would like to speak with a gastroenterologist, please contact us today to request an appointment.
1https://www.niddk.nih.gov/health-information/diagnostic-tests/endoscopic-retrograde-cholangiopancreatography
2https://www.uofmhealth.org/conditions-treatments/digestive-and-liver-health/bile-duct-stones
3https://www.ncbi.nlm.nih.gov/books/NBK539698/